Stronger Bones After 50 with the Right Habits
|
Reading time: 18 minutes
|
Key Takeaways
- Start Building Strong Bones Early: Osteoporosis happens when the body loses bone faster than it can replace it, especially after age 30. Healthy habits like weight-bearing exercises and eating calcium-rich foods early in life can help keep your bones strong and lower the risk of fractures as you get older.
- Prevention and Treatment Work Hand-in-Hand: Lifestyle changes, such as staying active, eating a balanced diet, and avoiding smoking or too much alcohol, are important for keeping bones healthy. For people already diagnosed with osteoporosis, treatments like bisphosphonates or denosumab can slow bone loss and strengthen bones when combined with these healthy habits.
- Detecting Osteoporosis Early Makes a Difference: Since osteoporosis often develops without symptoms, regular screenings like DEXA scans are important. Spotting warning signs like height loss or frequent fractures early allows for treatments and lifestyle changes that can slow the disease and improve quality of life.
Osteoporosis is a condition that weakens bones, making them fragile and more likely to break. It happens when the body loses too much bone, makes too little, or both. This condition affects millions of people worldwide and can make it harder to stay active and live independently.
One in three women and one in five men over the age of 50 are affected by osteoporosis, showing how common this condition is. Because it develops quietly, many people don’t realize they have it until a fracture occurs. These fractures can lead to lasting problems, including pain, reduced mobility, and challenges with daily life.
What is Osteoporosis?
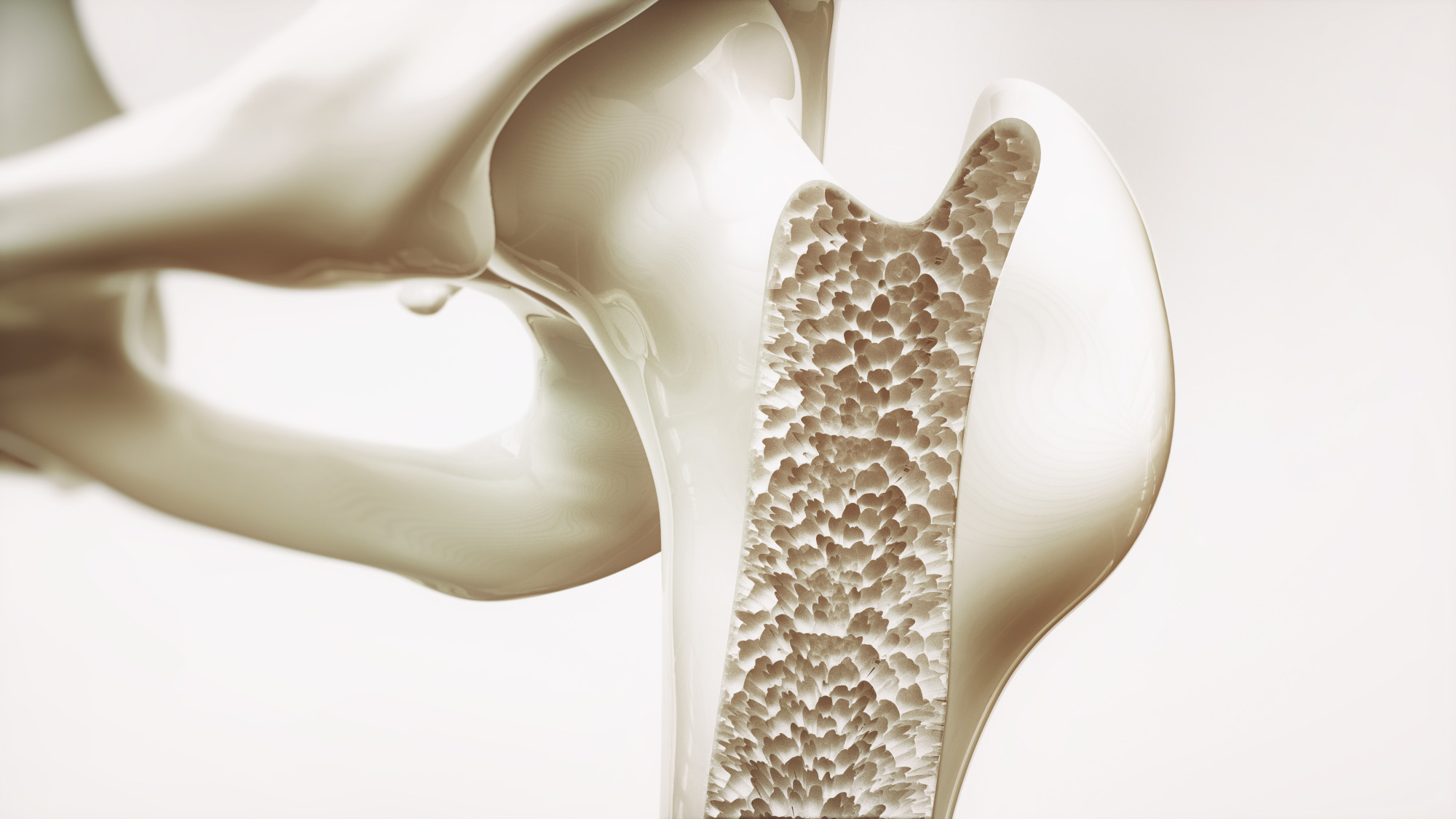
Osteoporosis is a condition that affects the strength and structure of bones, making them more fragile and prone to breaking. Bones are living tissue, constantly renewing themselves as the body replaces old bone with new, healthy bone to keep them strong and durable.
During young adulthood, the body builds bone faster than it loses it, and most people reach their strongest bones, or peak bone mass, by age 30. As people get older, this balance changes. The body starts losing bone faster than it can replace it. In people with osteoporosis, this process happens much quicker, making bones porous and brittle.
Weaker bones increase the risk of fractures, even from minor events like a small fall, a sudden twist, or even a strong sneeze. Commonly affected areas include the hips, spine, and wrists, which are important for daily activities and mobility.
Osteoporosis often develops without symptoms, which is why it’s sometimes called a “silent disease.” Over time, it can cause serious problems like chronic pain, a loss of height due to spinal fractures, or even hip fractures that might require surgery and long-term recovery.
Fortunately, treatments are available to slow bone loss and strengthen bones. Specific bone health medications, along with lifestyle changes like a better diet and regular exercise, can help manage osteoporosis and reduce the risk of fractures. Understanding this condition is an important first step toward protecting your bones and maintaining a healthier, more active life.
Risk Factors for Osteoporosis
Osteoporosis happens because of different factors that can weaken bones and reduce their strength. Knowing what increases the risk of osteoporosis can help people make better choices to protect their bones. These risk factors include changes in hormones, medical conditions, lifestyle habits, and inherited traits.
Hormonal Changes and Medical Conditions
Hormones play an important role in keeping bones healthy. In women, the hormone estrogen helps maintain strong bones. After menopause, estrogen levels drop, which causes bone loss to speed up. This is why postmenopausal women are more likely to have weak bones and fractures. For men, low levels of testosterone can also increase the risk of osteoporosis as they age.
Certain medical problems can also weaken bones. For example, an overactive thyroid speeds up bone loss. Autoimmune conditions like celiac disease or rheumatoid arthritis can interfere with how the body absorbs calcium or directly harm bone tissue. These health issues show how connected bone strength is to overall health.
Lifestyle and Nutrition Factors
Daily habits and diet have a big impact on bone strength. Being inactive for long periods, such as sitting too much, can weaken bones. Activities like walking, jogging, or lifting weights help bones stay strong by encouraging new growth.
Unhealthy habits, like smoking or drinking too much alcohol, also harm bones. Smoking damages the cells that build bone, while too much alcohol reduces the body’s ability to absorb calcium, a mineral that bones need to stay strong.
Eating enough calcium and protein is very important for bone health. Calcium is the building block of bones, while protein gives bones structure and support.
Foods like dairy products, green leafy vegetables, and fortified cereals are great sources of calcium. Protein can be found in lean meats, nuts, beans, and eggs. Without enough of these nutrients, bones can become weak and more likely to break.
Family History and Body Traits
Genetics also play a role in the risk of osteoporosis. If someone in your family has had osteoporosis or frequent fractures, you may be more likely to develop it too. Physical traits can also make a difference. People with smaller or thinner body frames often have lower bone mass, which increases their risk of bone loss as they age.
Body weight matters as well. Being underweight is linked to weaker bones, while being overweight can put extra pressure on bones, making fractures more likely. Knowing how these factors affect bone health can help people take steps to prevent problems.
Types of Osteoporosis
Osteoporosis is not the same for everyone. It can develop in different ways depending on a person’s age, gender, and overall health. There are two main types of osteoporosis: Type 1 and Type 2. Knowing the differences between them helps us understand their causes, effects, and who is most affected.
Type 1 Osteoporosis
Type 1 osteoporosis, also called postmenopausal osteoporosis, mostly affects women after menopause. It is closely linked to lower levels of a hormone called estrogen, which plays a key role in keeping bones strong. After menopause, estrogen levels drop, making it harder for the body to rebuild bones while bone loss speeds up.
This type of osteoporosis often leads to fractures in the wrists and spine. The spine is especially vulnerable, and fractures there can cause symptoms like back pain, a curved posture, or even a loss of height over time.
Wrist fractures are also common, often happening after minor falls. While men can develop Type 1 osteoporosis, it is much more common in women due to hormonal changes after menopause.
Type 2 Osteoporosis (Senile Osteoporosis)
Type 2 osteoporosis, often called senile osteoporosis, typically occurs after the age of 70 and affects both men and women. However, it is about twice as common in women, partly because women usually start with lower bone mass than men.
This type of osteoporosis happens because the body naturally loses its ability to maintain strong bones as it ages. Brittle bones caused by Type 2 osteoporosis often lead to fractures in the hips and other areas that carry weight, like the legs.
Hip fractures are especially serious and may require surgery and long recovery times. These injuries can also limit a person’s ability to move around independently.
Unlike Type 1, which mainly affects certain bones like the wrists and spine, Type 2 osteoporosis impacts a wider range of bones, making it a more general issue as people get older.
How to Prevent Osteoporosis
Preventing osteoporosis starts with building and keeping bones strong throughout life. By staying active, eating the right foods, and making healthy choices, you can lower the chances of losing bone density and reduce the risk of fractures. Taking action early helps bones stay strong as you age.
Weight-bearing and Strength Training Exercises
Exercise plays a big role in keeping bones healthy. Weight-bearing activities like walking, jogging, or dancing help bones grow stronger by putting pressure on them. This encourages the body to repair and build new bone tissue, keeping bones dense and strong over time.
Strength training is also very important. Exercises like lifting weights or using resistance bands target muscles and the bones that support them, making both stronger. Activities like yoga or tai chi improve balance and coordination, helping to prevent falls that could lead to fractures.
Making these activities part of your routine not only strengthens bones but also improves flexibility, balance, and mobility, helping you stay active and independent.
Nutrition for Bone Health
What you eat has a huge impact on your bones. Calcium is one of the most important nutrients for bone strength. It helps build and maintain bones. Good sources of calcium include low-fat dairy products like milk, cheese, and yogurt, as well as leafy green vegetables like spinach and kale. Fortified cereals and plant-based milks are also great options.
Vitamin D is just as important because it helps your body absorb calcium. Spending time in sunlight helps your body produce vitamin D, but you can also get it from foods like salmon, egg yolks, fortified milk, or orange juice.
Protein is another key nutrient for healthy bones. It provides the framework that bones need to grow and repair. Protein can be found in foods like lean meats, fish, eggs, nuts, beans, and tofu.
Including these nutrients in your daily diet helps your bones stay strong and reduces the risk of osteoporosis over time.
Healthy Lifestyle Habits
The choices you make every day can affect your bone health. Smoking damages the cells that build bone, making them weaker over time. Quitting smoking, no matter your age, helps protect your bones.
Alcohol can also harm bones. Drinking more than two alcoholic drinks a day can stop your body from absorbing enough calcium. Limiting alcohol helps keep bones stronger and supports overall health.
Maintaining a healthy weight is also important. Being underweight can lower bone density, while being overweight can strain bones, increasing the risk of fractures. A balanced diet and regular exercise help keep your weight in a healthy range, supporting strong bones.
Diagnosis and Early Detection
Osteoporosis often develops without obvious symptoms, making it hard to detect until a bone breaks. Recognizing the signs and identifying risk factors early can help manage the condition and lower the chances of fractures. Early detection involves understanding the symptoms and using medical tests to check bone health.
Screening and Testing
The first step in detecting osteoporosis is recognizing possible signs that your bones may be weaker than normal. One of the most common signs is a gradual loss of height over time, caused by the bones in the spine becoming compressed. Frequent fractures in areas like the hips, wrists, or spine—especially from minor accidents—can also indicate osteoporosis.
Doctors use specific tests to evaluate bone health and detect osteoporosis early. The most common test is a DEXA scan (Dual-Energy X-ray Absorptiometry), which measures bone density in important areas like the hips and spine. This test provides a clear picture of how strong your bones are and whether you might have osteoporosis.
Sometimes, doctors might use ultrasounds, usually on the heel, as an additional tool to check bone density. While less accurate than a DEXA scan, it can give a quick indication of bone health. Blood and urine tests may also be done to find out if there are other factors, like low calcium or vitamin D levels, contributing to bone loss.
With these tools, healthcare providers can make an accurate diagnosis and recommend the best treatments or lifestyle changes to slow or prevent further bone loss.
Importance of Early Detection
Catching osteoporosis early can make a big difference in how it affects your life. When detected early, people can take steps to slow bone loss and lower their risk of fractures. These steps might include improving their diet, doing more physical activity, or starting specific treatments that help strengthen bones.
Early diagnosis also helps doctors create a treatment plan tailored to the individual. For those with mild bone loss, small changes in diet and exercise might be enough. For people with more advanced bone loss, early detection means they can begin medications that may stop or even reverse bone damage.
Preventing fractures is another key benefit of early detection. Fractures from osteoporosis can lead to pain, difficulty moving, or the need for surgery. By addressing osteoporosis early, individuals can avoid these complications, maintain their independence, and continue living an active life.
Regular check-ups and timely testing give people the tools they need to manage osteoporosis and protect their bones over the long term. Taking action early helps ensure better outcomes and a higher quality of life.
Treatment Options for Osteoporosis
Osteoporosis treatments are designed to make bones stronger, reduce the chance of fractures, and slow down bone loss. Depending on the condition’s severity and a person’s overall health, different treatments can improve bone health and quality of life. These treatments include medications and hormone-based therapies.
Prescription Medications
Doctors often prescribe medications to help manage osteoporosis. These medicines work in different ways to slow bone loss or build bone strength.
- Fosamax (alendronate): This medication is part of a group called bisphosphonates. It slows the breakdown of bone tissue, allowing bones to stay dense or even regain some strength over time. Fosamax is usually taken as a weekly pill and is recommended for people at higher risk of fractures.
- Zoledronic acid: Another bisphosphonate, this medication is given through an annual infusion. It is a good option for people who prefer fewer treatments or have trouble taking pills. Zoledronic acid has been shown to reduce fractures in key areas like the hips and spine.
- Denosumab: This is a biological drug given as an injection every six months. It works by blocking a protein that causes bone loss, helping to maintain and strengthen bones. Denosumab is often prescribed for postmenopausal women at high risk of fractures or for those who haven’t responded well to other treatments.
These medications, combined with healthy lifestyle choices, can help individuals manage osteoporosis and protect their bones.
Hormone Replacement Therapy (HRT)
Hormone replacement therapy (HRT) may help women who are at high risk of osteoporosis, especially after menopause. HRT uses estrogen, or a combination of estrogen and progestin, to maintain bone density. Estrogen plays an important role in keeping bones strong, but its levels drop after menopause, leading to faster bone loss.
HRT can reduce the risk of fractures by preserving bone strength, especially during the early years of menopause when bone loss happens quickly. It is often recommended for women who haven’t responded to other osteoporosis treatments or who have severe menopausal symptoms along with bone loss.
However, HRT is not suitable for everyone. Doctors carefully evaluate a person’s health history and risks before prescribing it. In some cases, alternative treatments can provide similar benefits without hormone therapy.
Living with Osteoporosis
Living with osteoporosis means adopting healthy habits, following medical advice, and staying proactive about your health. While osteoporosis weakens bones and increases the risk of fractures, there are many practical ways to strengthen your bones, stay active, and improve your quality of life.
Practical Tips for Maintaining Bone Health
Taking care of your bones starts with making small, daily changes. Regular exercise helps strengthen bones and improve balance. Activities like walking, climbing stairs, or dancing are weight-bearing exercises that encourage new bone growth.
Yoga and tai chi are great for improving balance and coordination, which lowers the risk of falls. Strength training with light weights or resistance bands can also build muscle to support your bones.
Eating the right foods is just as important. Foods rich in calcium, like low-fat milk, cheese, yogurt, leafy greens, and calcium-fortified cereals, help maintain strong bones.
Vitamin D, which you can get from sunlight, fatty fish, egg yolks, or fortified milk, helps your body absorb calcium better. Protein is also key for bone strength and can be found in foods like lean meats, beans, nuts, and eggs.
Making your home safer is another way to prevent fractures. Remove tripping hazards like loose rugs, keep rooms well-lit, and consider adding grab bars in bathrooms to help prevent falls.
Regular Check-Ups and Following Treatment Plans
Managing osteoporosis requires regular visits to your doctor to check your bone health. Tests like DEXA scans help monitor bone density and show whether treatments are working. Doctors can adjust your treatment plan based on these results.
It’s also important to take any prescribed medications as directed. Medications like bisphosphonates or denosumab are most effective when taken on a regular schedule. Skipping doses or stopping medication without talking to your doctor can increase the risk of fractures.
If your doctor recommends supplements like calcium or vitamin D, make sure to include them in your daily routine.
Working with Healthcare Providers
Every person’s experience with osteoporosis is different, so it’s important to work with your doctor to create a plan that fits your needs. A doctor can recommend the best treatments based on your age, overall health, and the severity of your bone loss. For example, people at higher risk of fractures may need specific medications or physical therapy to improve strength and mobility.
Your doctor can also answer questions about exercise, diet, or any concerns about managing osteoporosis. Staying in regular contact with your healthcare provider ensures that you are taking the right steps to protect your bones and feel confident in managing your condition.
Frequently Asked Questions (FAQ)
Osteoporosis often brings up many questions about what it is and how to manage it. Below are some common questions and clear answers to help you better understand bone health.
What Are the First Signs of Osteoporosis?
Osteoporosis is sometimes called a “silent disease” because it develops without obvious symptoms. However, there are warning signs to watch for:
- Height loss: Gradual shrinking may happen as small fractures in the spine cause it to compress.
- Posture changes: A hunched back or slouching may signal weakened bones.
- Frequent fractures: Breaking bones in the hips, wrists, or spine from minor falls or injuries could be a sign of fragile bones.
- Persistent back pain: Weakened spine bones may collapse, causing ongoing discomfort.
If you notice these signs, it’s important to talk to a doctor about your bone health.
How Effective Are Bone Health Medications?
Medications for osteoporosis are very effective when taken as directed. They work in two main ways:
- Slowing bone loss: Medications like Fosamax (a bisphosphonate) help reduce the breakdown of bone tissue, keeping bones denser and stronger.
- Building new bone: Treatments like denosumab block signals that cause bone loss, allowing bones to strengthen over time.
Some medications, like zoledronic acid, are given as an annual infusion, while others, like denosumab, are taken as injections every six months. These options are convenient for those who prefer fewer doses.
While medications cannot fully “cure” osteoporosis, they lower the risk of fractures and help people maintain an active, independent lifestyle. Success depends on taking medications as prescribed and combining them with healthy habits like exercise and a nutrient-rich diet.
Can Osteoporosis Be Reversed?
Osteoporosis cannot be completely reversed, but its progression can often be slowed, and bone density may improve in some cases. Treatments such as bisphosphonates, denosumab, and hormone replacement therapy (HRT) are designed to:
- Strengthen bones
- Lower fracture risk
- Encourage bone repair
Lifestyle changes also play an important role. Activities like walking, yoga, and weight-bearing exercises promote bone growth and overall health. Eating foods rich in calcium, getting enough vitamin D, and staying active can make a big difference.
While complete reversal is rare, combining treatments and healthy habits can help reduce the impact of osteoporosis.
What Lifestyle Changes Have the Biggest Impact on Bone Health?
Simple changes in daily habits can make a big difference for your bones:
- Exercise regularly: Activities like walking, dancing, and jogging strengthen bones by encouraging bone growth. Strength training with light weights or resistance bands helps build muscles that support bones.
- Eat for strong bones: Include calcium-rich foods such as dairy, leafy greens, and fortified cereals in your diet. Add vitamin D from fatty fish, egg yolks, or sunlight to help your body absorb calcium. Protein from lean meats, beans, or nuts supports the structure of bones.
- Avoid harmful habits: Smoking damages bone cells, and too much alcohol weakens bones and increases fall risks. Quitting smoking and limiting alcohol can significantly improve bone health.
By making these lifestyle changes, you can actively protect your bones and lower the risk of fractures caused by osteoporosis.
Conclusion
Osteoporosis is a condition that can affect anyone, but there are ways to reduce its impact and protect your bones. By learning about the risks, recognizing early warning signs, and making healthy choices, you can take steps to keep your bones strong and maintain your quality of life.
Preventing and managing osteoporosis starts with identifying risk factors like family history, lifestyle habits, or a lack of important nutrients. Regular check-ups and screenings, such as DEXA scans, help detect osteoporosis early so treatment can begin when it’s most effective.
Healthy habits are key to managing osteoporosis. Eating foods rich in calcium and vitamin D, staying active with weight-bearing exercises like walking or lifting light weights, and avoiding harmful habits like smoking or heavy drinking can make a big difference. These steps not only help prevent osteoporosis but also support medical treatments for those already diagnosed.
For those needing extra help, medications can slow bone loss and make bones stronger. There are affordable treatment options available, and working with a healthcare provider ensures your plan is right for you. Exploring these options can give you confidence in managing osteoporosis. To find affordable medication solutions, check our prices.
Information provided on this website is for general purposes only. It is not intended to take the place of advice from your practitioner







